caregiver video story board
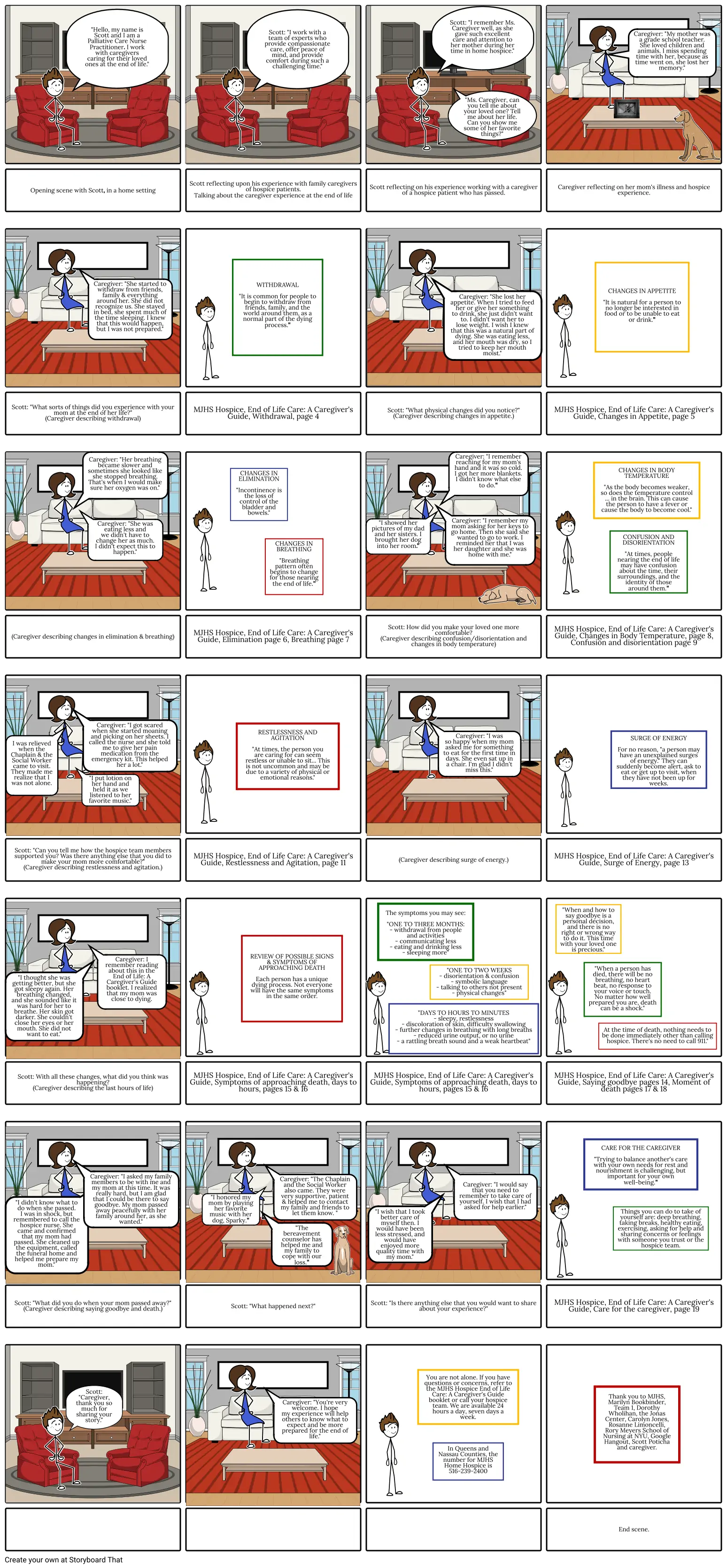
Storyboard Text
- "Hello, my name is Scott and I am a Palliative Care Nurse Practitioner. I work with caregivers caring for their loved ones at the end of life."
- Scott: "I work with a team of experts who provide compassionate care, offer peace of mind, and provide comfort during such a challenging time."
- Scott: "I remember Ms. Caregiver well, as she gave such excellent care and attention to her mother during her time in home hospice."
- "Ms. Caregiver, can you tell me about your loved one? Tell me about her life. Can you show me some of her favorite things?"
- Caregiver: "My mother was a grade school teacher. She loved children and animals. I miss spending time with her, because as time went on, she lost her memory."
- Opening scene with Scott, in a home setting
- Caregiver: "She started to withdraw from friends, family & everything around her. She did not recognize us. She stayed in bed, she spent much of the time sleeping. I knew that this would happen, but I was not prepared."
- Scott reflecting upon his experience with family caregivers of hospice patients. Talking about the caregiver experience at the end of life
- WITHDRAWAL "It is common for people to begin to withdraw from friends, family, and the world around them, as a normal part of the dying process."
- Scott reflecting on his experience working with a caregiver of a hospice patient who has passed.
- Caregiver: "She lost her appetite. When I tried to feed her or give her something to drink, she just didn't want to. I didn't want her to lose weight. I wish I knew that this was a natural part of dying. She was eating less, and her mouth was dry, so I tried to keep her mouth moist."
- Caregiver reflecting on her mom's illness and hospice experience.
- CHANGES IN APPETITE "It is natural for a person to no longer be interested in food or to be unable to eat or drink."
- Scott: "What sorts of things did you experience with your mom at the end of her life?" (Caregiver describing withdrawal)
- Caregiver: "Her breathing became slower and sometimes she looked like she stopped breathing. That's when I would make sure her oxygen was on."
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Withdrawal, page 4
- CHANGES IN ELIMINATION "Incontinence is the loss of control of the bladder and bowels."
- Scott: "What physical changes did you notice?" (Caregiver describing changes in appetite.)
- Caregiver: "I remember reaching for my mom's hand and it was so cold. I got her more blankets. I didn't know what else to do."
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Changes in Appetite, page 5
- CHANGES IN BODY TEMPERATURE "As the body becomes weaker, so does the temperature control ... in the brain. This can cause the person to have a fever or cause the body to become cool."
- (Caregiver describing changes in elimination & breathing)
- Caregiver: "She was eating less and we didn't have to change her as much. I didn't expect this to happen."
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Elimination page 6, Breathing page 7
- CHANGES IN BREATHING "Breathing pattern often begins to change for those nearing the end of life."
- "I showed her pictures of my dad and her sisters. I brought her dog into her room."
- Scott: How did you make your loved one more comfortable? (Caregiver describing confusion/disorientation and changes in body temperature)
- Caregiver: "I remember my mom asking for her keys to go home. Then she said she wanted to go to work. I reminded her that I was her daughter and she was home with me."
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Changes in Body Temperature, page 8, Confusion and disorientation page 9
- CONFUSION AND DISORIENTATION "At times, people nearing the end of life may have confusion about the time, their surroundings, and the identity of those around them."
- I was relieved when the Chaplain & the Social Worker came to visit. They made me realize that I was not alone.
- Caregiver: "I got scared when she started moaning and picking on her sheets. I called the nurse and she told me to give her pain medication from the emergency kit. This helped her a lot."
- "I put lotion on her hand and held it as we listened to her favorite music."
- RESTLESSNESS AND AGITATION "At times, the person you are caring for can seem restless or unable to sit... This is not uncommon and may be due to a variety of physical or emotional reasons."
- Caregiver: "I was so happy when my mom asked me for something to eat for the first time in days. She even sat up in a chair. I'm glad I didn't miss this."
- SURGE OF ENERGY For no reason, "a person may have an unexplained surges of energy." They can suddenly become alert, ask to eat or get up to visit, when they have not been up for weeks.
- "I thought she was getting better, but she got sleepy again. Her breathing changed, and she sounded like it was hard for her to breathe. Her skin got darker. She couldn't close her eyes or her mouth. She did not want to eat."
- Scott: "Can you tell me how the hospice team members supported you? Was there anything else that you did to make your mom more comfortable?" (Caregiver describing restlessness and agitation.)
- Caregiver: I remember reading about this in the End of Life: A Caregiver's Guide booklet. I realized that my mom was close to dying.
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Restlessness and Agitation, page 11
- REVIEW OF POSSIBLE SIGNS & SYMPTOMS OF APPROACHING DEATH Each person has a unique dying process. Not everyone will have the same symptoms in the same order.
- (Caregiver describing surge of energy.)
- The symptoms you may see: "ONE TO THREE MONTHS: - withdrawal from people and activities - communicating less - eating and drinking less - sleeping more"
- "ONE TO TWO WEEKS - disorientation & confusion - symbolic language - talking to others not present - physical changes"
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Surge of Energy, page 13
- "When and how to say goodbye is a personal decision, and there is no right or wrong way to do it. This time with your loved one is precious."
- "When a person has died, there will be no breathing, no heart beat, no response to your voice or touch. No matter how well prepared you are, death can be a shock."
- Scott: With all these changes, what did you think was happening? (Caregiver describing the last hours of life)
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Symptoms of approaching death, days to hours, pages 15 & 16
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Symptoms of approaching death, days to hours, pages 15 & 16
- "DAYS TO HOURS TO MINUTES - sleepy, restlessness - discoloration of skin, difficulty swallowing - further changes in breathing with long breaths - reduced urine output, or no urine - a rattling breath sound and a weak heartbeat"
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Saying goodbye pages 14, Moment of death pages 17 & 18
- CARE FOR THE CAREGIVER "Trying to balance another's care with your own needs for rest and nourishment is challenging, but important for your own well-being."
- At the time of death, nothing needs to be done immediately other than calling hospice. There's no need to call 911."
- "I didn't know what to do when she passed. I was in shock, but remembered to call the hospice nurse. She came and confirmed that my mom had passed. She cleaned up the equipment, called the funeral home and helped me prepare my mom."
- Scott: "What did you do when your mom passed away?" (Caregiver describing saying goodbye and death.)
- Caregiver: "I asked my family members to be with me and my mom at this time. It was really hard, but I am glad that I could be there to say goodbye. My mom passed away peacefully with her family around her, as she wanted."
- Scott: "What happened next?"
- "I honored my mom by playing her favorite music with her dog, Sparky."
- "The bereavement counselor has helped me and my family to cope with our loss."
- Caregiver: "The Chaplain and the Social Worker also came. They were very supportive, patient & helped me to contact my family and friends to let them know. "
- Scott: "Is there anything else that you would want to share about your experience?"
- "I wish that I took better care of myself then. I would have been less stressed, and would have enjoyed more quality time with my mom."
- Caregiver: "I would say that you need to remember to take care of yourself. I wish that I had asked for help earlier."
- MJHS Hospice, End of Life Care: A Caregiver's Guide, Care for the caregiver, page 19
- Things you can do to take of yourself are: deep breathing, taking breaks, healthy eating, exercising, asking for help and sharing concerns or feelings with someone you trust or the hospice team.
- Scott: "Caregiver, thank you so much for sharing your story."
- Caregiver: "You're very welcome. I hope my experience will help others to know what to expect and be more prepared for the end of life."
- You are not alone. If you have questions or concerns, refer to the MJHS Hospice End of Life Care: A Caregiver's Guide booklet or call your hospice team. We are available 24 hours a day, seven days a week.
- In Queens and Nassau Counties, the number for MJHS Home Hospice is 516-239-2400
- Thank you to MJHS, Marilyn Bookbinder, Team 1, Dorothy Wholihan, the Jonas Center, Carolyn Jones, Rosanne Limoncelli, Rory Meyers School of Nursing at NYU, Google Hangout, Scott Poticha and caregiver.
-
- End scene.
Over 30 Million Storyboards Created

