Unknown Story
Storyboard Text
- .
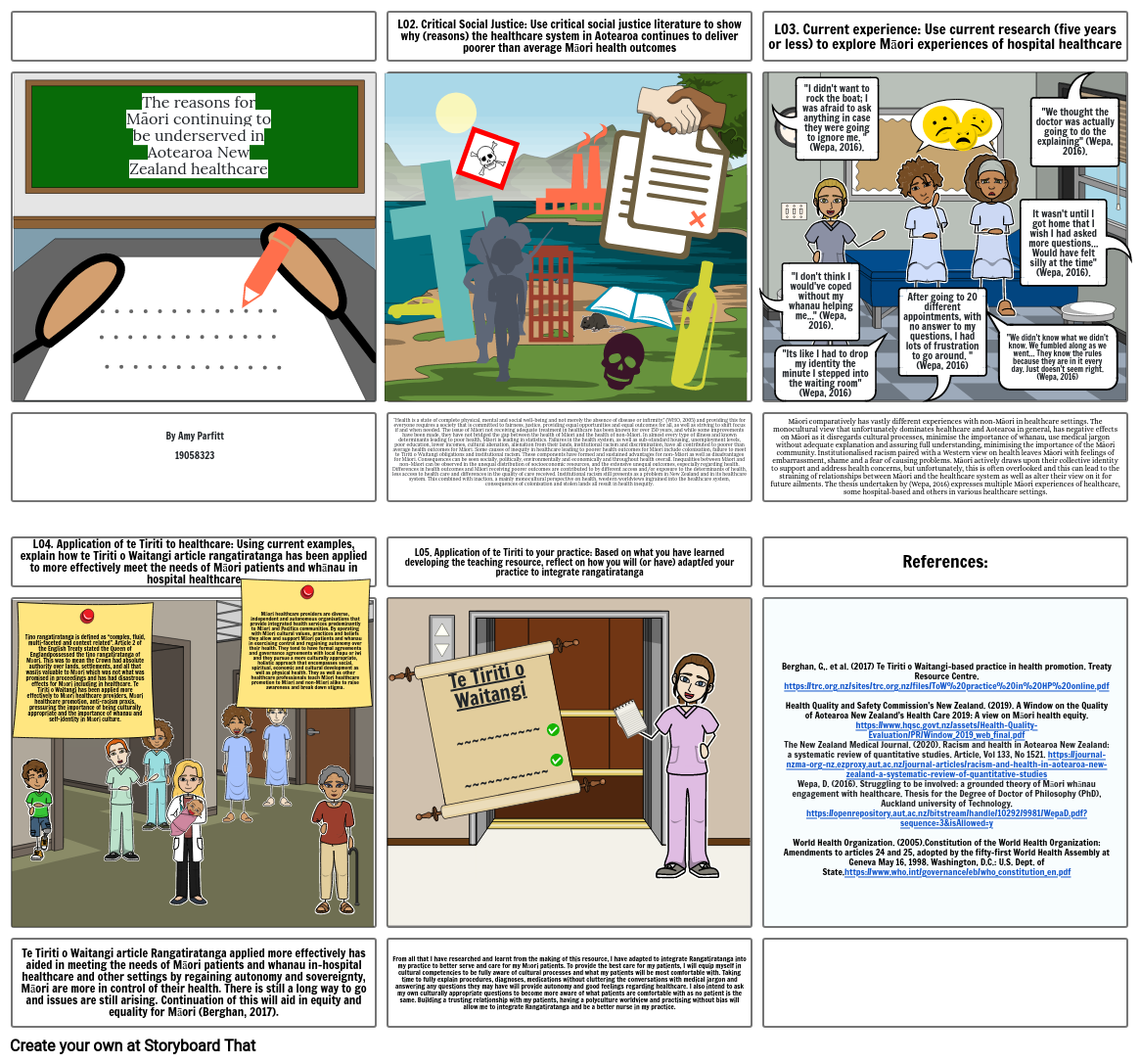
- The reasons for Māori continuing to be underserved in Aotearoa New Zealand healthcare
- LO2. Critical Social Justice: Use critical social justice literature to show why (reasons) the healthcare system in Aotearoa continues to deliver poorer than average Māori health outcomes
- "I don't think I would've coped without my whanau helping me..." (Wepa, 2016).
- LO3. Current experience: Use current research (five years or less) to explore Māori experiences of hospital healthcare
- "I didn't want to rock the boat; I was afraid to ask anything in case they were going to ignore me. "(Wepa, 2016).
- "Its like I had to drop my identity the minute I stepped into the waiting room" (Wepa, 2016)
- After going to 20 different appointments, with no answer to my questions, I had lots of frustration to go around. "(Wepa, 2016)
- .
- "We didn't know what we didn't know. We fumbled along as we went... They know the rules because they are in it every day. Just doesn't seem right. (Wepa, 2016)
- It wasn't until I got home that I wish I had asked more questions... Would have felt silly at the time" (Wepa, 2016).
- "We thought the doctor was actually going to do the explaining" (Wepa, 2016).
- ..
- LO4. Application of te Tiriti to healthcare: Using current examples, explain how te Tiriti o Waitangi article rangatiratanga has been applied to more effectively meet the needs of Māori patients and whānau in hospital healthcare
- Tino rangatiratanga is defined as “complex, fluid, multi-faceted and context related”. Article 2 of the English Treaty stated the Queen of England possessed the tino rangatiratanga of Māori. This was to mean the Crown had absolute authority over lands, settlements, and all that was/is valuable to Māori which was not what was promised in proceedings and has had disastrous effects for Māori including in healthcare. Te Tiriti o Waitangi has been applied more effectively to Māori healthcare providers, Māori healthcare promotion, anti-racism praxis, pressuring the importance of being culturally appropriate and the importance of whanau and self-identity in Māori culture.
- By Amy Parfitt 19058323
- Māori healthcare providers are diverse, independent and autonomous organisations that provide integrated health services predominantly to Māori and Pacifica communities. By operating with Māori cultural values, practices and beliefs they allow and support Māori patients and whanau in exercising control and regaining autonomy over their health. They tend to have formal agreements and governance agreements with local hapu or iwi and they pursue a more culturally appropriate, holistic approach that encompasses social, spiritual, economic and cultural development as well as physical health. They as well as other healthcare professionals teach Māori healthcare promotion to Māori and non-Māori alike to raise awareness and break down stigma.
- “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” (WHO, 2005) and providing this for everyone requires a society that is committed to fairness, justice, providing equal opportunities and equal outcomes for all, as well as striving to shift focus if and when needed. The issue of Māori not receiving adequate treatment in healthcare has been known for over 150 years, and while some improvements have been made, they have not bridged the gap between the health of Māori and the health of non-Māori. In almost every type of illness and known determinants leading to poor health, Māori is leading in statistics. Failures in the health system, as well as sub-standard housing, unemployment levels, poor education, lower incomes, cultural alienation, alienation from their lands, institutional racism and discrimination, have all contributed to poorer than average health outcomes for Māori. Some causes of inequity in healthcare leading to poorer health outcomes for Māori include colonisation, failure to meet te Tiriti o Waitangi obligations and institutional racism. These components have formed and sustained advantages for non-Māori as well as disadvantages for Māori. Consequences can be seen socially, politically, environmentally and economically and throughout health overall. Inequalities between Māori and non-Māori can be observed in the unequal distribution of socioeconomic resources, and the extensive unequal outcomes, especially regarding health. Differences in health outcomes and Māori receiving poorer outcomes are contributed to by different access and/or exposure to the determinants of health, less access to health care and differences in the quality of care received. Institutional racism still presents as a problem in New Zealand and in its healthcare system. This combined with inaction, a mainly monocultural perspective on health, western worldviews ingrained into the healthcare system, consequences of colonisation and stolen lands all result in health inequity.
- LO5. Application of te Tiriti to your practice: Based on what you have learned developing the teaching resource, reflect on how you will (or have) adapt/ed your practice to integrate rangatiratanga
- Te Tiriti o Waitangi~~~~~~~~~~~~~~~~~~~~~~
- Māori comparatively has vastly different experiences with non-Māori in healthcare settings. The monocultural view that unfortunately dominates healthcare and Aotearoa in general, has negative effects on Māori as it disregards cultural processes, minimise the importance of whanau, use medical jargon without adequate explanation and assuring full understanding, minimising the importance of the Māori community. Institutionalised racism paired with a Western view on health leaves Māori with feelings of embarrassment, shame and a fear of causing problems. Māori actively draws upon their collective identity to support and address health concerns, but unfortunately, this is often overlooked and this can lead to the straining of relationships between Māori and the healthcare system as well as alter their view on it for future ailments. The thesis undertaken by (Wepa, 2016) expresses multiple Māori experiences of healthcare, some hospital-based and others in various healthcare settings.
- References:
- Berghan, G,. et al. (2017) Te Tiriti o Waitangi-based practice in health promotion. Treaty Resource Centre. https://trc.org.nz/sites/trc.org.nz/files/ToW%20practice%20in%20HP%20online.pdfHealth Quality and Safety Commission's New Zealand. (2019). A Window on the Quality of Aotearoa New Zealand’s Health Care 2019: A view on Māori health equity. https://www.hqsc.govt.nz/assets/Health-Quality-Evaluation/PR/Window_2019_web_final.pdfThe New Zealand Medical Journal. (2020). Racism and health in Aotearoa New Zealand: a systematic review of quantitative studies. Article, Vol 133, No 1521. https://journal-nzma-org-nz.ezproxy.aut.ac.nz/journal-articles/racism-and-health-in-aotearoa-new-zealand-a-systematic-review-of-quantitative-studiesWepa, D. (2016). Struggling to be involved: a grounded theory of Māori whānau engagement with healthcare. Thesis for the Degree of Doctor of Philosophy (PhD), Auckland university of Technology. https://openrepository.aut.ac.nz/bitstream/handle/10292/9981/WepaD.pdf?sequence=3&isAllowed=yWorld Health Organization. (2005).Constitution of the World Health Organization: Amendments to articles 24 and 25, adopted by the fifty-first World Health Assembly at Geneva May 16, 1998. Washington, D.C.: U.S. Dept. of State.https://www.who.int/governance/eb/who_constitution_en.pdf
- Te Tiriti o Waitangi article Rangatiratanga applied more effectively has aided in meeting the needs of Māori patients and whanau in-hospital healthcare and other settings by regaining autonomy and sovereignty, Māori are more in control of their health. There is still a long way to go and issues are still arising. Continuation of this will aid in equity and equality for Māori (Berghan, 2017).
- From all that I have researched and learnt from the making of this resource, I have adapted to integrate Rangatiratanga into my practice to better serve and care for my Māori patients. To provide the best care for my patients, I will equip myself in cultural competencies to be fully aware of cultural processes and what my patients will be most comfortable with. Taking time to fully explain procedures, diagnoses, medications without cluttering the conversations with medical jargon and answering any questions they may have will provide autonomy and good feelings regarding healthcare. I also intend to ask my own culturally appropriate questions to become more aware of what patients are comfortable with as no patient is the same. Building a trusting relationship with my patients, having a polyculture worldview and practising without bias will allow me to integrate Rangatiratanga and be a better nurse in my practice.
- .
Over 30 Million Storyboards Created

